This website offers guidance for building a Learning Health System (LHS), focusing on tools, models and frameworks that might be helpful. However, it is not a “how to” guide. Indeed, there is no model for building an LHS that can be “lifted and shifted”. LHSs are complex by nature, and must be co-designed with local stakeholders.
We aim to refresh “The Potential of Learning Healthcare Systems” [1] which was published in 2015. Here, we supplement the interviews and workshops conducted for that report with five new expert workshops, a purposeful literature review and six more years of experience building LHSs.
Figure A provides a framework for thinking about the components of an LHS and this is mirrored by the sections of the report. This first section describes how a group of stakeholders might determine their Rationale for developing an LHS (the outer ring of Figure A). The next section discusses the Technical Building Blocks of an LHS (the hub of Figure A). Next, we explain why Understanding and Managing Complexity in an LHS is about more than just technology (the ring marked ‘Complexity’). The final main section explains the key Strategic Considerations in an LHS (the ring second from the outside).
An LHS can operate at any scale, from a team to a small provider organisation, or from a regional group of organisations to a national or even international system. [2] The elements considered in this report are relevant at each scale, as illustrated by Figure A.
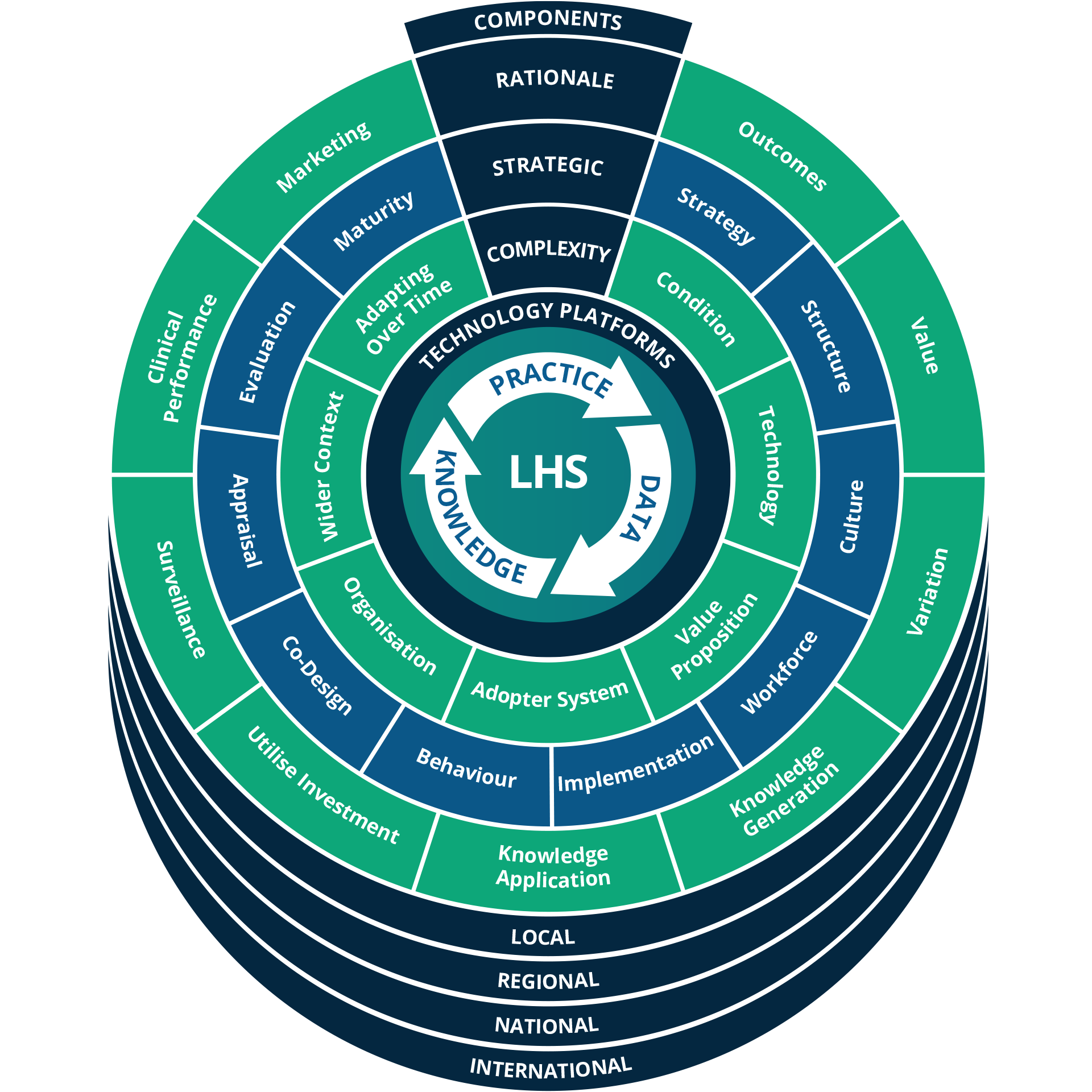
Figure A The Learning Health System Framework.
What is a Learning Health System, and why would you want one?
Many years before the concept was applied to healthcare, a learning organisation was defined as “an organization skilled at creating, acquiring, and transferring knowledge, and at modifying its behaviour to reflect new knowledge and insights” [3].
The idea was introduced to healthcare in 2007 by the United States Institute of Medicine (IoM, now the National Academy of Medicine) [4], which later defined it as a system in which “science, informatics, incentives, and culture are aligned for continuous improvement and innovation, with best practices seamlessly embedded in the delivery process, [with] patients and families active participants in all elements, and new knowledge captured as an integral by-product of the delivery experience” [5].
On the face of it, the definitions above are comprehensive, but not very specific. Almost any health system can claim to be a Learning Health System, in that there are scientific processes, informatics and incentives in play. Knowledge is usually captured in some form or other, and most systems at least claim to seek improvement. However, there are few, if any systems in which these elements are fully aligned for continuous improvement and innovation.
Importantly, the focus is on collecting data to generate knowledge and applying it to improve practice (the hub of Figure A).
In most cases, data come from Electronic Health Records, clinical registries or other routinely collected sources. Data are analysed by communities of practice or by a range of quantitative methods, often devised by academic health centres, public bodies or commercial organisations [6]. The knowledge generated is then used to change practice by informing deliberative processes or by directly feeding decision support systems.
Learning Health Systems have been called many different things, including data hubs, living labs, innovation or informatics hubs, learning networks, learning laboratories, community-clinician participatory data healthcare research, data driven improvement initiatives, interventional informatics, practice-based data networks, circular data-driven healthcare, Learning Healthcare Systems and Rapid Learning Health Systems[6].
It is important to recognise that a Learning Health System is an ongoing journey rather than a destination; the very concept of a Learning Health System is that there is always something new to learn [7]. They conduct similar activities regardless of scale, giving them a fractal property. This means that many elements will be reusable as Learning Health Systems scale up. Figure A shows that each of the elements considered in this report can be co-designed at the local, regional, national and international level.
There is necessarily an interdisciplinary science developing around the Learning Health System concept [8], evidenced by the formation of new university departments [9], conferences [10] and an academic journal [11].
There is necessarily an interdisciplinary science developing around the Learning Health System concept [8], evidenced by the formation of new university departments [9], conferences [10] and an academic journal [11].
The rationale for developing a Learning Health System often includes some or all of the following, which were explored in more detail in the earlier Learning Healthcare Project report [1]:
To improve patient outcomes and experience:
While most health systems seek to improve the quality and safety of care, many fail even to measure comprehensive and robust outcomes. A Learning Health System with the ability to deliver actionable knowledge to the point of care could enable improvements to patient outcomes and experience [12].
To provide better value healthcare:
Patient outcome and patient-level costing data can enable Value Based Healthcare Delivery [13]. This may reduce the cost for a given outcome – in other words, doing things right. Perhaps more fundamentally, a Learning Health System can inform priorities for resource allocation – doing the right things.
To reduce unjustified variation:
A Learning Health System can identify variations in outcomes and in the availability of health interventions by geography or by subpopulation. It can highlight health inequalities or positive deviants, and apply behaviour change methods to address such variations [14].
To generate generalisable knowledge:
A Learning Health System can empower research. It can help identify potential participants for traditional randomised controlled trials. It can enable low-cost monitoring or long-term follow-up of participants, by tracking when they interact with the health system. It can host prospective pragmatic trials or retrospective observational studies. It can generate evidence that is relevant to small sub-populations or those with comorbidities or polypharmacy [15], and can deliver evidence for policymaking at the population-level.
To optimise the use of knowledge and evidence for decision making:
A Learning Health System can improve the use of research evidence, staff knowhow, learning from experience and organisational memory. It can close the loop by delivering knowledge back to the front-line, in a form that is likely to be acted upon. It can also monitor the impact of that action.
To identify and track epidemiological phenomena in near real-time:
The Covid-19 pandemic has highlighted the importance of real-time health surveillance systems. These can be developed on top of the infrastructure required to support other Learning Health System functions [16]
To maximise the benefits of technological innovation and investment:
Many health systems have invested vast resources into Electronic Health Records (EHR) and other Health IT infrastructure. Without investment in something like a Learning Health System, EHRs often represent little more than a clunky version of paper notes. A Learning Health System can exploit the newly available data and increase the value of existing Health IT infrastructure.
To expand the education, training and performance of clinicians:
A Learning Health System can enable performance feedback and personalised professional development using routinely collected clinical data [17].
Marketing (Because it sounds good):
In some cases, the Learning Health System concept has been used as a marketing label, applied to existing systems. This is due to the vagueness of the definitions above. It risks diluting and discrediting the concept, but it can have benefits. If it provides a set of organising principles for existing activities, it can point the way to more strategic future developments.
Check out our latest report on Realising the Potential of Learning Health Systems
This website also contains links to other Learning Health System Projects around the world.
